CINCINNATI – For women considering a hysterectomy to treat cervical cancer, a large new study sheds surprising light on the options: The less-invasive procedure doesn’t improve your chance of survival over the more-extensive operation.
The study says more research is needed about the seemingly counterintuitive conclusion. But the results could change how cervical cancer is treated in the United States.
“What’s interesting is that in no other study for any other cancer or any other benign condition have we ever found worse overall survival rates for minimally invasive surgical options,” said Dr. Daniel Margul of the University of Cincinnati Medical Center, the study’s co-author.
The study was published Wednesday in the New England Journal of Medicine, one of the nation’s most prestigious publications on medical science. Margul worked on the study as a medical student at Northwestern University. He earned his medical degree in May then started his medical residency at UCMC this summer. He's working the overnight shift at the moment.
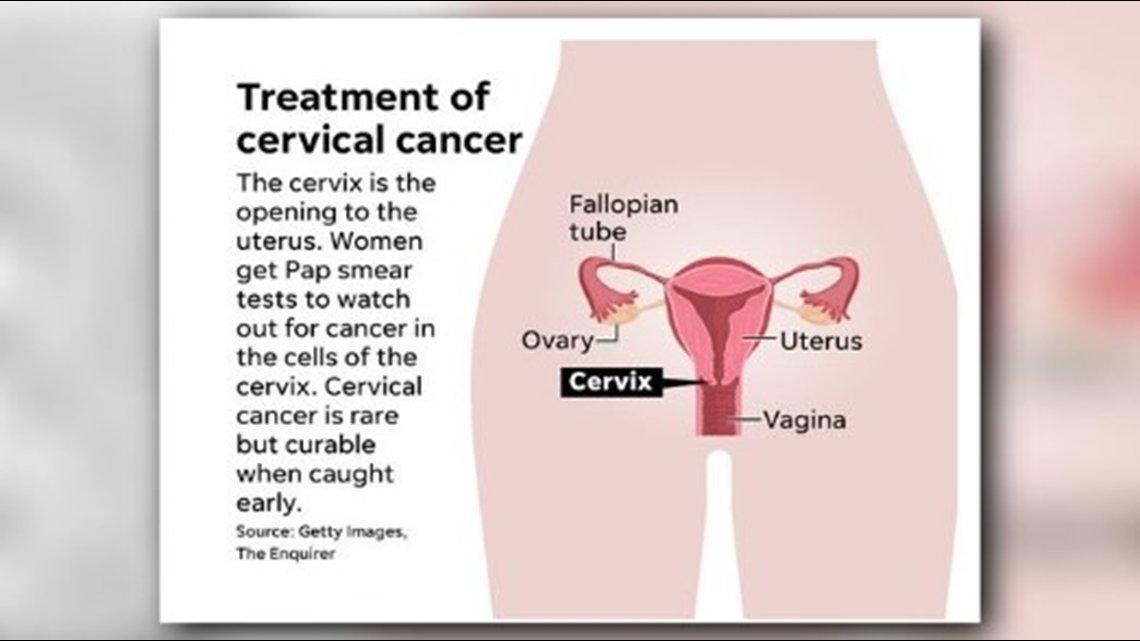
Cervical cancer once was a major cause of death for American women of childbearing years. In the 1950s, the acceptance of the Pap smear test to catch cervical cancer early rapidly brought down death rates in the developed world. Still, more than 450 Ohioans die of cervical cancer every year.
When cervical cancer is caught early, it’s treatable and curable, most often with a radical hysterectomy to remove the uterus, surrounding ligaments, the cervix and a portion of the vagina. For years, the procedure involved an abdominal incision and a hospital stay.
In 2006, doctors began offering a “minimally invasive” hysterectomy with smaller incisions and faster recovery, and the procedure became popular. Margul said the study found about 60 percent of hysterectomies for cervical cancer were done in that manner.
The study released Wednesday is the first time survival rates have been measured for the two surgical methods with a large enough population and the time span to produce results useful to doctors and patients.
“There weren’t enough cases to do a large national database study until 2010,” Margul said, “and then you want at least four or five years of follow-up. A lot of single institutions had tried to put together their cases, but they didn’t have big enough numbers.”
The study published Wednesday looked at 2,461 women treated between 2010 and 2013. About half underwent the less-invasive procedure. The startling result: The four-year death rate was 9.1 percent among women who had minimally invasive surgery and 5.3 percent among those who had the traditional surgery.

The difference was big enough to pull down the nation’s overall survival rate for cervical cancer for the same four years, the study reported.
The study was done at Massachusetts General Hospital in Boston, Northwestern University in Evanston, Illinois, MD Anderson Cancer Center in Houston and Columbia University in New York City.
Margul said the study’s researchers do not know the reasons for the higher death rates among women who chose the minimally invasive procedure. The surgery is “technically demanding,” and surgeons may not be taking enough tissue. The procedure also requires plumping the abdomen with carbon dioxide to create room to operate, and the gas has been shown in earlier research to make cervical cancer cells more active or grow in number, Margul said.